AHA Medical/Scientific
Statement
State-of-the-Art Review
Improving Survival From Sudden Cardiac
Arrest: The "Chain of Survival" Concept
A Statement for Health Professionals From
the Advanced Cardiac Life Support Subcommittee and the Emergency Cardiac Care Committee,
American Heart Association.Writing Group
Richard O. Cummins, MD, MPH, MSc; Joseph P. Ornato, MD;
William H. Thies, PhD; and Paul E. Pepe, MD
Committee Members
John E. Billi, MD; James Seidel, MD, PhD; Allan S. Jaffe, MD;
Loring S. Flint, MD; Sidney Goldstein, MD;
Norman S. Abramson, MD; Charles Brown, MD; Nisha C. Chandra, MD;
Edgar R. Gonzalez, PharmD, RPh; Lawrence Newell, EdD, NREMT-P;
Kenneth R. Stults, MS, PAC; and George E. Membrino, PhD
Overview
More people can survive sudden cardiac arrest when a particular sequence of events occurs
as rapidly as possible. This sequence is 1) recognition of early warning signs, 2)
activation of the emergency medical system, 3) basic cardiopulmonary resuscitation, 4)
defibrillation, 5) intubation, and 6) intravenous administration of medications. The
descriptive device "chain of survival" communicates this understanding is a
useful way (Figure 1). While separate specialized programs
are necessary to develop strength in each link, all of the links must be connected.
Weakness in any link lessens the chance of survival and condemns the efforts of an
emergency medical services (EMS) system to poor results. The chain of survival concept has
evolved through several decades of research into sudden cardiac arrest. Effective system
interventions have been identified that will allow survivors to remain neurologically
intact. While a few urban systems may be approached the current practical limit for
survivability from sudden cardiac arrest, most EMS systems, both in the United States and
other countries, have defects in their chain. Poor resuscitation rates have been the rule.
This statement describes the research supporting each link and recommends specific actions
to strengthen the chain of survival.
"Improving Survival From Sudden Cardiac Arrest: The 'Chain of Survival' Concept"
was approved by the American Heart Association SAC/Steering Committee on October 17, 1990.
Requests for reprints should be sent to the Office of Scientific Affairs, American Heart
Association, 7320 Greenville Avenue, Dallas, TX 75231.
The Links in the Chain of Survival
The Early Access Link
The chain of survival begins with early access, in which the patient is helped as quickly
as possible. Early access includes the implied component of early recognition. The
resuscitation chain is initiated when a medical emergency is recognized and the emergency
medical system accessed and activited.1 The time required for access begins the moment an emergency is
recognized, by either the person with symptoms or a witness to the emergency. With sudden
cardiac arrest, access time begins at the moment of collapse, and includes recognition of
the emergency, the decision to make the call, time spent locating a telephone and
emergency number, interrogation of the caller by the emergency dispatcher, and the
decision to send an emergency vehicle. The dispatcher may need additional times to route
the call to the proper response station or vehicle (call-processing time). Once the
responder is notified, ambulance response time begins. Ambulance response time is the
interval from receipt of the call by the emergency responder to arrival of emergency
personnel at the scene. Additional time may elapse before the responder actually examines
the patient. Recognition, call processing, and ambulance response time add seconds,
typically minutes, to the critical interval between arrest and initiation of emergency
treatment.
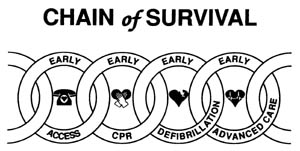
Figure 1. Sequence of events in emergency cardiac care is displayed
schematically by "chain of survival" metaphor.
The most common approach to shorten the interval between
collapse and arrival of emergency personnel has been to acquire more ambulances,2,3 which
is both expensive and inefficient, especially if the EMS system is established. Studies
have shown that after a certain point an increase in the number of ambulances fails to
lower response time significantly.4 In one model, response time varied inversely as the square root of
the number of vehicles per square mile; an 80% increase in the number of vehicles reduced
average response time by only 1 minute.4 This same 1-minute reduction in average response time could be
achieved by greater public awareness and more efficient dispatching systems, and at far
less cost.
The early access link can be strengthened through public education, especially persons
most likely to witness a cardiac arrest, and by installation of an efficient emergency
communication system. Educational and public service programs such as those of the
American Heart Association1 and the American Red Cross5 are designed to
make the public aware of what to do when cardiac arrest occurs. Participants in classes on
cardiopulmonary resuscitation (CPR) and AHA-sponsored schoolsite and worksite training
learn the warning signs of heart attack, how to recognize a person in cardiac arrest, and
to quickly call the EMS system when a person collapses. Persons who are uninformed about
chest pain and respiratory distress may not comprehend signs of an impending cardiac
arrest. When a person collapses, such a witness may wait a long time before calling the
emergency dispatch center. A witness may telephone neighbors, relatives, or even his or
her personal physician before calling the emergency number, as observed in both central
London6 and rural Iowa.7 In Belgium and Holland it is almost the rule to first call the
local physician. This poses a problem in terms of early defibrillation because physicians
are less likely to carry defibrillators than emergency responders. In Iowa a "phone
first" program has been started to achieve immediate notification of the EMS system
when a person collapses.7 Such educational campaigns may become more widespread. Early
access ensures that precious minutes are not wasted at the start of cardiac arrest.
Lack of a three-digit 999 emergency dispatch system (or its equivalent) can produce
confusion and delays because witnesses may call the wrong number, call multiple numbers,
or spend time searching for the number. In one community in North Carolina, 85 different
emergency numbers are listed in the local telephone book.8,9 In contrast, in
Seattle, Washington, which has an enhanced 911 system, 90% of 1,271 people interviewed
identified 999 as their EMS notification number.10 Investigators
from Minneapolis who performed a before-and-after evaluation of a 911 system11 noted
that the percentage of emergency callers who could activate the EMS system in less than a
minute rose from 63% before implementation of the system to 82% afterward. The percentage
of callers who made only one telephone call to activate the system went from 40% before
the 911 system was started to 74% after the system began.
Another study showed that imprecise knowledge of how to notify the emergency system can
cause confusion and delays.12 In this telephone survey, people living in 999 system communities
knew the correct number to call 85% of the time; in regional systems with several fire
department operating from one dispatching center, people knew the correct number to call
only 47% of the time; in systems with a local seven-digit number for a particular fire
district, people gave the correct number only 36% of the time. Many people who lived near
a 999 area thought 999 was their emergency number; when they mistakenly called 999, delays
of 30 seconds to 2 minutes resulted. Establishment of a 999 emergency system is a key
step. Given the transient and mobile nature of today's population, a universal access
number must be adopted by EMS systems. By 1992 a common emergency telephone number will be
introduced in the European community and will cover a population of more than 350 million.
The Early CPR Link
The next link in the chain of survival is early initiation of basic CPR.1,13 Basic
CPR should be started immediately after cardiac arrest is recognized and should coincide
with efforts to gain access to and activate the EMS system. EMS systems should rely on
trained citizens rather than emergency responders to initiate CPR. With rare exceptions,
initiation of CPR by emergency personnel is too late. Only systems with rapid response
times, such as that in Milwaukee, Wisconsin,14,15 can employ EMS providers as the primary initiators of CPR.
For almost 3 decades the chest compressions and positive pressure ventilations of standard
CPR have helped return pulseless, nonbreathing patients to spontaneous respiration and
cardiac perfusion.16,17 The value of early CPR is that it can buy time for the primary
cardiac arrest patient1,13,18-22 by producing enough blood flow to the central nervous system and
the myocardium to maintain temporary viability. To do so, however, basic CPR must be
started early, and the earlier the better. Initial CPR must be followed by rapid
defibrillation, intubation, and administration of cardiovascular medications by EMS
personnel.23 Early bystander CPR is less helpful in resuscitation if EMS
personnel equipped with the defibrillator arrive late, or about 8-12 minutes after
collapse.24 Recent data from the Belgium Cardio-Pulmonary-Cerebral
Resuscitation Registry18 and Scotland,25 however, suggest some prolonged benefit from bystander CPR even
with late arrival of advanced live support personnel. The combination of late CPR (more
than 4 minutes) and late advanced life support (more than 12 minutes) is particularly
lethal.22,24,26 Several researchers have called these time dimensions the
resuscitation "failure zone."27
Many reports contain data to compare the survival rates of cardiac arrest victims who
receive early CPR (defined as citizen-initiated CPR) with the survival rates of those who
receive late CPR (defined as emergency responder-initiated CPR).22,24,28,29-42 Table 1 presents summary data from these studies, including
estimated odds ratios for survival. Early CPR usually differs from late CPR by about 4
minutes. In all but one system, researchers observed a positive benefit of early CPR when
they compared survival rates between persons who received early CPR and those who received
late CPR. The magnitude of this contribution may be considerable since the odds ratios for
improved survival with early CPR can range as high as 11.5 (Table 1).
In Milwaukee,14,36 the only system in which this benefit was not observed, emergency
personnel performed late CPR an average interval of only 2 minutes after early
bystander-initiated CPR. Thus the data from Milwaukee simply compare early CPR with even
earlier CPR. The similar survival rates for people who received bystander CPR compared
with those deprived of bystander CPR are not surprising and provide additional support for
the concept of a narrow window of CPR effectiveness.38 The association
between early CPR and improved survival appears related to the effect of basic CPR on
ventricular fibrillation.18,38,43,44 Researchers have observed that when rescuers start CPR early, the
patient is more likely to be in ventricular fibrillation when a monitoring unit arrives.44
Investigators in King County, Washington, observed that 80% of cardiac arrest victims were
in ventricular fibrillation/ventricular tachycardia if they had received early bystander
CPR, compared with 68% if they had received delayed CPR.38 In Stockholm, 67%
of people in cardiac arrest in whom CPR was started by bystanders were in ventricular
fibrillation/ventricular tachycardia, whereas only 45% of persons not given bystander CPR
were in ventricular fibrillation/ventricular tachycardia.43 The Belgian
Cardio-Pulmonary-Cerebral Resuscitation Registry has reported a 42% prevalence of
ventricular fibrillation in cardiac arrest patients who received bystander CPR, compared
with 29% in arrest patients who received delayed CPR.18
These three studies suggest that CPR prolongs the duration of ventricular fibrillation. In
addition, they suggest that the presence of ventricular fibrillation operates as a
dependent variable rather than an independent variable in analyses of survival data.18,22
Victims who receive early CPR are also more likely after electrical shock to convert to a
cardiac rhythm associated with restoration of spontaneous circulation.22,26,38
In King County, Washington, persons in ventricular fibrillation when EMS personnel arrived
has a 37% rate of long-term survival if they were given bystander CPR, compared with 29%
if they were not.38 In Houston, 40% of patients with ventricular
fibrillation/ventricular tachycardia were discharged from the hospital if they had
received bystander CPR, versus 19% for such patients not given bystander CPR.22
Several approaches ensure the performance of basic CPR by bystanders before emergency
responders arrive. The most widely advocated is citizen CPR training. Community-based CPR
training programs, endorsed and conducted by the American Heart Association and the
American Red Cross, have trained millions of laypersons in CPR.1 The American Heart
Association has suggested that if 20% of adults were trained in CPR, morbidity and
mortality from out-of-hospital cardiac arrest might be significantly reduced.45 Some
communities have actually achieved this level of adult training, despite physician
reluctance to "prescribe" CPR training for family members and friends of
high-risk patients.10,46,47 In the Seattle area, for example, Leonard Cobb and coworkers48
have trained over 2 million people. In Minneapolis a survey of 2,310 adults noted that 23%
were trained in CPR.49
However, there are problems with the concept that a threshold level of citizen training
can be "protective." Most people trained in CPR never see an arrest; most people
who see an arrest have not been trained in CPR.49,50 The Minneapolis survey found that
only 10% of the population trained in CPR had witnessed a cardiac arrest49 and only 30% of
witnesses to a cardiac arrest had been trained in CPR. Only 19% of persons trained in
Minneapolis continued retraining every year.49 This figure nearly duplicates that in a
report by Gombeski,50 who noted that only 21% of their trainees returned for 1-year
retraining.
Other data, however, suggest a more positive picture.51-54 Eisenberg et
al51 observed that some knowledge of CPR techniques is so prevalent
that many citizens attempt CPR without formal training. In addition, they perform CPR
despite a high prevalence of disagreeable physical characteristics (the presence of
saliva, blood, or emesis) encountered during performance of bystander CPR.52 Cobb et
al53,54 observed that outcomes for CPR by untrained citizens is similar to
outcomes for trained laypersons. The Belgian Cardio-Pulmonary-Cerebral Resuscitation
Registry has noted that the quality of bystander CPR is difficult to evaluate.55 In
Belgium the most common bystander CPR errors were omission of mouth-to-mouth ventilations,
which occurred 46% of the time, and omission of chest compressions, which occurred 17% of
the time.55 Outcomes were significantly better when rescuers performed both
ventilations and chest compressions, compared with ventilations alone or compressions
alone.55
|
| Table 1. Controlled Studies of Survival
(Discharged Alive) From Out-of-Hospital Cardiac Arrest: Bystander Cardiopulmonary
Resuscitation Compared with Late Cardiopulmonary Resuscitation |
|
| Location/System |
Witnessed arrest |
Rhythm |
Number of
patients |
Discharged
alive (n) |
Odds ratio* |
|
| 1. |
Oslo, Norway28
EMTs only |
Not reported |
Not reported |
Bys CPR=75
Late CPR=556 |
36% (27)
8% (43) |
6.7 |
| 2. |
Birmingham29
Paramedics only |
Implied yes |
VF or VT |
Bys CPR=7
Late CPR=12 |
86% (6)
50% (6) |
6.0 |
| 3. |
Seattle30
EMTs and paramedics |
76% overall witnessed |
VF only |
Bys CPR=109
Late CPR=207 |
43% (47)
21% (43) |
2.9 |
| 4. |
Winnipeg31
EMTs only |
Not reported |
VF or VT |
Bys CPR=65
Late CPR=161 |
25%
(16) |
6.2 |
| 5. |
Iceland32
EMTs only |
Not reported |
All rhythms |
Bys CPR=38
Late CPR=84 |
42% (16)
2% (2) |
11.5 |
| 6. |
Vancouver33
EMTs and paramedics |
77% overall witnessed |
All rhythms |
Bys CPR=43
Late CPR=272 |
21% (9) |
4.0 |
| 7. |
Los Angeles34
Paramedics |
41% overall witnessed |
All rhythms
VF only |
Bys CPR=93
Late CPR=150
Bys CPR=45
Late CPR=70 |
22% (20)
5% (7)
27% (12)
6% (4) |
5.6
6.0 |
| 8. |
King County13
EMTs and paramedics |
Not reported |
All rhythms |
Bys CPR=108
Late CPR=379 |
23% (25)
2% (45) |
2.2 |
| 9. |
Pittsburgh35
Paramedics |
Not reported |
VF/VT only |
Bys CPR=25
Late CPR=59 |
24% (6)
7% (4) |
4.3 |
| 10. |
Milwaukee36
EMTs and paramedics |
Witnessed only |
All rhythms
Coarse VF |
Bys CPR=1,248
Late CPR=252
Bys CPR=628
Late CPR=151 |
15% (182)
15% (38)
24% (148)
23% (35) |
1.0
1.0 |
| 11. |
Michigan/Ohio37
communities (EMTs
and paramedics) |
Not reported |
All rhythms |
Bys CPR=472
Late CPR=1,367 |
13% (56)
5% (64) |
2.7 |
| 12. |
King County38
EMT-Ds and paramedics |
Both
Witnessed only |
All rhythms
All rhythms |
Bys CPR=726
Late CPR=1,317
Bys CPR=579
Late CPR=718 |
27% (196)
13% (177)
32% (186)
22% (158) |
2.4
1.7 |
| 13. |
York/Adams, Pa.39
EMTs and paramedics |
Witnessed only |
VF only |
Bys CPR=157
Late CPR=225 |
22% (34)
6% (13) |
4.5 |
| 14. |
Tucson, Ariz.40
EMTs and paramedics |
Witnessed only |
All rhythms |
Bys CPR=65
Late CPR=130 |
20% (13)
9% (12) |
2.5 |
| 15. |
West Yorkshire42
Ambulance personnel |
Not reported |
All rhythms |
Bys CPR=47
Late CPR=50 |
15% (7)
8% (4) |
2.0 |
| 16. |
Belgium41
Ambulance Personnel |
Not reported |
All rhythms |
Bys CPR=985
Late CPR=2,036 |
10% (98)
5% (109) |
1.9 |
| 17. |
Houston22
EMTs and medics |
Both |
Unmonitored VF/VT |
Bys CPR=53
Late CPR=133 |
30% (16)
14% (19) |
2.1 |
|
EMT, emergency medical technician; EMT-D, emergency
medical technician trained to defibrillate; VF, ventricular fibrillation; VT, ventricular
tachycardia; Bys, bystander; CPR, cardiopulmonary resuscitation.
*Odds ratio is not a simple ratio of survival rates. It is calculated as the odds of
surviving with bystander CPR (number discharged alive divided by number who die) divided
by the odds of discharge alive for people who received late CPR (number discharged alive
divided by number who die). |
|
Another approach to early CPR is the concept of targeted CPR training.10,53,54,56-59 Such programs are for persons who have an increased likelihood of
having to perform CPR, including middle-aged persons, residents and staff of senior
centers, survivors of myocardial infarction, and family members of persons identified as
having cardiac arrest risk factors. These programs are slowly becoming more widespread and
represent an important change in the focus of CPR training. Much CPR training in the
United States focuses on the young, especially school-age children and young adults,57 who are
easy to train and show energetic interest. However, they are not likely to witness a
cardiac arrest or to take a CPR course. They do, of course, become the "future"
performers of CPR as they enter the age group where risk increases. Cardiac arrest victims
are typically aging men, who live at home6,18,60 and are usually poorly educated and nonprofessional.61 In King
County, Washington, the average age of cardiac arrest patients is 65 years; 77% of cardiac
arrests happen at home, and 75% of the victims are men.60,62 Therefore,
persons with the highest likelihood of witnessing a cardiac arrest and being called upon
to perform CPR are those living with or closely associated with middle-aged men.
Regardless of age, the prognosis for persons resuscitated from cardiac arrest, even the
elderly (those over 70 years old), is excellent.63,64 Unfortunately,
few middle-aged women in the United States have received formal CPR training, and those
who have received training seldom live with high-risk patients.10,11 In one survey
of people trained to perform CPR, only 7% lived with family members known to have heart
disease.10
A final method to achieve early CPR is dispatcher-assisted CPR instruction, programs in
which emergency telephone dispatchers offer CPR instructions to persons who call to report
a cardiac arrest.51,54-67 Delivery of instructions and performance of a complete CPR cycle
of 15 chest compressions and 2 ventilations can be accomplished in 3-4 minutes,51,65,67
even by persons who have never received CPR training. Telephone instruction also improves
the quality of CPR performed by persons with prior CPR training in manikin simulations.22,67
Panicked bystanders can be calmed and directed by dispatchers and encouraged to perform
CPR, despite their alarm at the sudden sight of a loved one who is cyanotic and
breathless. With this program, plus other educational efforts, the percent of cardiac
arrests in which CPR was initiated by bystanders in King County, Washington, has increased
from 30% in 1980 to 60% in 1988 (unpublished data).
The Early Defibrillation Link
The purpose of early defibrillation is to reestablish a normal spontaneous rhythm in the
heart. Several new approaches can help achieve early defibrillation:
- Automated defibrillators used by the first responding
emergency personnel
- Automated defibrillators used by community responders, that
is, persons whose usual occupation or training does not require responding to emergencies.
- Home defibrillation programs for high-risk patients
- Transtelephonic defibrillation
The rationale for early defibrillation emerges from data
that demonstrate that almost 85% of persons with ambulatory, out-of-hospital, primary
cardiac arrest experience ventricular tachyarrhythmias during the early minutes after
collapse.
68
In one report 157 ambulatory (not hospitalized) patients experienced fatal arrhythmias
during continuous cardiac monitoring.68 The initial dysrhythmia in 62% of patients was ventricular
tachycardia that quickly evolved to ventricular fibrillation, in 8% the dysrhythmia was
primary ventricular fibrillation, and in 13% it was torsades de pointes. The duration of
the ventricular tachycardia that preceded the ventricular fibrillation ranged from a few
seconds to several minutes. This study involved a select population of patients who had
some indication for ambulatory cardiac monitoring. Nevertheless, the rhythms they
experienced are probably representative of the usual initial rhythms of the sudden cardiac
arrest victim.
In prehospital studies, the rhythm of arrest cannot be identified until emergency
personnel arrive with a defibrillator/monitor, 4-8 minutes later. In these studies the
percent of people in ventricular tachyarrhythmias was lower, at 60% of less.22,62 Most
eventual survivors emerge from the group of people who remain in ventricular fibrillation
when emergency personnel arrive. For example, in King County, Washington, over 92% of
cardiac arrest survivors were from this group,62 and over 80% in
Houston.22
Additional evidence about the importance of early defibrillation comes from cardiac arrest
experiences in supervised cardiac rehabilitation programs. On the rare occasion when a
person in such a program experiences cardiac arrest, it is witnessed, CPR is started
immediately, and defibrillation is performed within minutes. Fletcher and Cantwell69
reported five cardiac arrests in a medically supervised exercise program; all were
resuscitated. Haskell70 reported that among 13,570 patients in 30 exercise centers, 50
cardiac arrests occurred and 42 (84%) were resuscitated. Hossack and Hartwig71
observed 2,464 people in a supervised cardiac rehabilitation program over a 13-year
period. In this group 25 men suffered a cardiac arrest, and all 25 (100%) were
successfully resuscitated. Van Camp and Peterson72 summarized the
experience in 167 cardiac rehabilitation programs; 21 cardiac arrests occurred, and
personnel resuscitated 18 (86%) without neurologic sequelae. The type of rhythm at arrest
in these series was not reported, but sudden arrest during exercise suggests that the
large majority of these patients were in ventricular fibrillation. Overall, of 101 cardiac
arrests in these reports, staff members resuscitated 90 (89%) of the victims. This is the
highest survival rate reported among defined population groups, and it confirms the value
of immediate efforts in early CPR and defibrillation.
In England, general practitioners, the most frequent responders to patients with chest
pain and cardiac arrest, have observed that early defibrillation alone produces successful
resuscitations.73 Many patients in Britain call their general practitioner during
the early stages of a myocardial infarction. About 5% of these patients experience a
cardiac arrest after the physician arrives.74,75 The British Heart Foundation donated 78 defibrillators to 25
general practices and reported on the experiences after 1 year.73 A total of 19
patients suffered cardiac arrest in the presence of a general practitioner who had a
defibrillator: 13 (68%) were in ventricular fibrillation, nine were successfully
resuscitated outside the hospital, and six were discharged from the hospital.73
In the earliest prehospital programs,33-35,42,76-86 only paramedics provided defibrillation. In most studies of
paramedic-only systems, the time between collapse and arrival of paramedics averaged more
than 12 minutes. These programs therefore generally provide what is more correctly termed late
defibrillation.
Consequently, the reported survival rates for these systems have been modest, ranging from
7% to 18% for all rhythms.87 Researchers in the early 1980s demonstrated the ability of
personnel less well trained than paramedics, namely, emergency medical technicians (EMTs),
to successfully use defibrillators.88-91 Early defibrillation programs implemented for firefighters and
minimally trained EMS first responders spread slowly, more often because of implementation
barriers and administrative inertia than from doubt of clinical efficacy.92,93
The proposals to allow less well trained emergency personnel to operate defibrillators
initially provoked controversy, but most concerns have since disappeared. Conceptually,
early defibrillation programs represented the transfer of what was a medical act –
diagnosis of the rhythm and operation of a defibrillator – into the hands of
nonphysicians. Some authorities accepted the transfer of skills to paramedics. However,
many authorities hesitated to permit defibrillation by less well trained emergency
personnel. Rational reasons for this hesitancy vanished by the late 1980s with widespread
acceptance of the principle of early defibrillation1,20,23 and the
success of automated external defibrillators.94,95 Regrettably, in Germany, France, Japan, and other countries,
medicolegal factors still prevent implementation of early defibrillation programs by
nonphysicians.
The principle of early defibrillation holds that the professional rescuer who arrives
first at the scene of a cardiac arrest should carry a defibrillator and be trained to
operate it.1,20,23 With few exceptions, the defibrillator should be automated and
external.93,94,96-102 Automated external defibrillators are highly accurate98,99,101-103 and eliminate the need for training in the complex skills of
rhythm recognition. The operator simply attaches the defibrillator's adhesive electrodes
to the chest of the person thought to be in cardiac arrest. When activated by a single
control, the device analyzes the rhythm, and if ventricular fibrillation or tachycardia is
present, the device either charges and delivers a shock (automatic devices) or indicates
to the operator that a shock is needed (semiautomatic, or shock-advisory, devices).104,105
With shock-advisory devices, the operator delivers the shock by pushing a second control.104,106
This simplicity of operation decreases the time and expense of initial training and
continuing education and markedly increases the number of persons who can operate the
devices. Clinical studies also show that systems using automated defibrillators can
deliver the first shock up to 1 minute faster than conventional defibrillators because of
the speed with which these devices can be attached and with which they operate.98,99
Each year more communities in the United States allow the use of both automated and
conventional defibrillators by EMTs and by less trained personnel call first responders,
a term that refers specifically to persons who have completed a 40-hour course. The term
can refer to a much larger group of public safety employees, including firefighters,
ambulance personnel, part-time emergency volunteers, police officers, highway patrol
personnel, security guards, merchant marine sailors, and airline, railroad, and other
public transportation vehicle crews.
Automated defibrillators are used by first responders around the world,107,108
with early defibrillation programs in Scotland,25 Denmark,109
England,6 West Berlin,107,108 Norway,110 Sweden,43 Australia,111 Singapore,112 Finland, Belgium, and many other countries. By 1988, 37 states in
the United States had passed legislation permitting early defibrillation by EMTs and, in
some states, basic first reponders.113 An additional 10 states planned to initiate similar programs in
1989.113 Many communities permit first-responder (usually firefighter)
defibrillation, including Houston; Dallas; Memphis; San Francisco; Salt Lake City;
Seattle; King County, Washington; and Eugene-Springfield, Oregon.102,114-116 The
International Association of Fire Chiefs has endorsed this concept and has started an
initiative called RapidZap,114-116 which has the goal of equipping all fire department emergency
response vehicles with automated defibrillators by the year 2000. The fire chiefs adopted
this concept not only out of concern to provide effective care for all citizens but also
concern for the well-being of their personnel. Surveys of firefighter deaths have noted
that the majority of on-duty deaths are due to sudden cardiac arrest.117,118
How effective are programs in which defibrillators are given to EMTs and first responders?
Variable degrees of success have been observed in clinical studies thus far. The published
survival rates for systems whose prehospital response teams consist only of EMTs trained
in defibrillation range from 6% to 26% for patients found to be in ventricular
fibrillation.43,88,89,119-121 The most important comparison, however, is between the survival
rate in communities before and after institution of an early defibrillation program. In
suburban communities in King County, Washington, for example, the survival rate for
patients in ventricular fibrillation increased from 7% to 26%.88 Similarly, in
communities in Iowa it increased from 3% to 19%.90 In southeastern
Minnesota the survival rate was 4% without EMT defibrillation and 17% with such a program,119
whereas in northeastern Minnesota the survival rate was 2.5% without and 9.9% with EMT
defrillation.77 When an early defibrillation program was started in certain
Wisconsin communities, the survival rate rose from 3.6% to 6.4% for all cardiac arrests
and was 11% for patients initially noted to be in ventricular fibrillation (Table 2),122 It is important to note that these programs should maintain and
increase initial improvements in survival rates as experience and competency improve over
time.
|
| Table 2. Effectiveness of Early Defibrillation
Programs: Survival From Ventricular Fibrillation |
|
| Location |
Before early
defibrillation |
After early
defibrillation |
Odds ratio for
improved survival* |
| King County88 |
7% (4/56) |
26% (10/38) |
4.6 |
| Iowa90 |
3% (1/31) |
19% (12/64) |
6.9 |
Southeastern
Minnesota119 |
4% (1/27) |
17% (6/36) |
5.2 |
Northeastern
Minnesota77 |
3% (3/118) |
10% (8/81) |
4.2 |
| Wisconsin122 |
4% (32/893) |
11% (33/304) |
3.3 |
|
| *The odds ratio is not a simple ratio of survival rates.
It is calculated as the odds of surviving after an early defibrillation program (number
who live divided by number who die), divided by the odds of surviving before an early
defibrillation program (number who live divided by number who die). |
Home and community responder defibrillation programs.
Two other techniques advocated to help achieve early defibrillation are home
defibrillation programs for high-risk patients and early defibrillation by community
responders. Community responders include public safety workers or laypersons who may have
a perceived duty to respond to an emergency.96,123-125 Although these approaches have been under evaluation for several
years, their specific effects on community-wide survival rates from cardiac arrest have
not been determined.123 Moore et al126 observed that of 95 survivors of ventricular fibrillation, only 63
(66%) were eligible for a home defibrillator, and only 38 of 47 (81%) persons approached
agreed to participate. This suggests that approximately half (0.66x0.81) of ventricular
fibrillation survivors would receive the device and appropriate training. McDaniel et al127 also
experienced recruitment problems in a similar home-defibrillation study. Only 8% of
survivors of acute myocardial infarction participated in their study. The reasons for low
participation included patients living alone, patients discharged to nursing homes,
patients having no telephone, resuscitation considered medically inappropriate,
implantation of automatic internal defibrillators, residence outside the study areas, no
perceived chance of repeat cardiac arrest, religious objections, and elimination from the
study at the demand of personal physicians.126,127
Nevertheless, enough experience has accumulated to establish the feasibility of training
family members of high-risk patients and community responders to use automated
defibrillators.126-129 Despite some decline in skill retention and performance, family
members and lay responders can remember most training and retain the skill for up to 1
year and can use the device at the moment of cardiac arrest of a family member or
coworker.128
So far, only limited clinical experience demonstrates the practicality and effectiveness
of home and community responder defibrillation programs. Chadda et al130
reported a case series of 30 patients with witnessed cardiac arrest. Lay persons used
automated defibrillators before the arrival of trained emergency personnel. Rescuers
resuscitated eight of these patients to an organized rhythm associated with spontaneous
circulation. Five were discharged from the hospital. Swenson et al131 reported a
series of 48 high-risk patients where the research team trained family members to operate
automated defibrillators. Five cardiac arrests occurred in this series. The trained home
responders used the automated defibrillator four times, and three patients had successful
restoration of circulation.
Researchers from King County, Washington, however, have experienced less positive results
with home132 and community responder defibrillation.128 Eisenberg et al132 placed
automated defibrillators in the homes of 59 persons who had survived prehospital cardiac
arrest. Ten cardiac arrests occurred; home responders used the device in six patients.
Only two patients were in ventricular fibrillation. One of the two patients was
resuscitated but survived only a few months with residual neurological deficits. In
another King County study, researchers placed 14 automated defibrillators in a variety of
community settings and trained 146 lay people working in those settings to operate the
device.128 Only three cardiac arrests occurred. Recognition and operation
errors prevented proper attachment and use of the defibrillator for all three patients.
However, manufacturers have since developed simpler, lighter, and more sophisticated
automated defibrillators with more user-friendly protocols and simpler placement of
electrode pads. Researchers may achieve better results if they conduct future studies with
the currently available devices.
In contrast, several other studies have achieved better results when automated
defibrillators were placed with community responders. Weaver et at133 trained 160
security personnel at the 1986 World's Exposition in Vancouver, British Columbia, to
operate an automated defibrillator in the event of a cardiac arrest. There were five
cardiac arrests among 22.1 million visitors. Rescuers used automated external
defibrillation on each victim, two of whom were in ventricular fibrillation. Automated
external defibrillation was successful in both patients, and sustained circulation
returned. Both patients were moving and semiconscious by the time emergency personnel
arrived. In England researchers placed automated external defibrillators on long-distance
aircraft of an international air carrier.134 This preliminary study ceased when another company purchased the
air carrier, but senior cabin attendants trained with great enthusiasm. Several other
airlines are likely to implement similar programs in the near future. In London
researchers trained conductors at several British Rail stations to operate automated
defibrillators. There are early anecdotal reports of successful resuscitation.134
High-risk or isolated industrial settings represent another interesting target group for
implementation of early defibrillation programs. Safety personnel have, for example,
placed and successfully used automated external defibrillators on oil platforms in the
North Sea, at electricity plants, and on passenger cruise ships and merchant marine
vessels.95,100,110,130
Future research will help establish the exact role of these innovative approaches.
However, clinical evidence is insufficient to support widespread home placement of
automated external defibrillators with high-risk patients. The evidence is more
encouraging for busy public places such as airports, railway stations, convention centers,
major hotels, and large public assemblies, and high-risk or remotely located industries
with trained safety personnel.
Transtelephonic defibrillation. Transtelephonic defibrillation is a recently
introduced method to provide early defibrillation.135-137 However, it
should not be classified with automated external defibrillation. In transtelephonic
defibrillation a trained family member or other companion attaches adhesive
monitor/defibrillator pads to a person with cardiac complaints or in cardiac arrest. The
defibrillator pads are attached through cables to a home unit that then transmits the
rhythm by telephone circuitry (either hard-wired or cellular) to a remote base station.
Emergency personnel at the base station interpret the rhythm and make the decision to
deliver a shock. Base station controls can be used to charge the home defibrillator unit
and deliver the shock. A two-way speaker phone provides simultaneous voice communication
between the home and the base station.
Researchers have confirmed this concept of remote defibrillation in hospital settings.136,137
Physicians have attached the device to patients in one hospital location (usually a
coronary care unit for elective cardioversions) and operated it from another. This
approach offers potential advantages over automated external defibrillators when used in
the home setting, including two-way voice communication, automatic dialing of 911, and
transfer of decision making to emergency personnel.138 Although
approved for clinical use, clinical experience confirming the effectiveness of prehospital
transtelephonic defibrillation is limited to a single patient, widely reported in the lay
press.139 It remains to be seen whether transtelephonic defibrillation will
be considered cost-effective and put to major practical use. This doubt is especially
valid since clinicians have already confirmed the ability of automated external
defibrillators to interpret rhythms and deliver shocks satisfactorily.
The Early Advanced Cardiac Life Support Link
In many instances CPR and defibrillation alone do not achieve or sustain resuscitation.
The unique interventions of the early advanced cardiac life support link –
endotracheal intubation and intravenous medication – are necessary to further improve
the chances of survival. In the United States, paramedics provide advanced cardiac life
support for prehospital cardiac arrest patients.140 Paramedics
receive 1,000-3,000 hours of classroom training and field instruction and can provide
intubation, defibrillation, and intravenous medications.
EMS systems in other countries provide many models of care. Some are more innovative than
those used in the United States. There are no paramedics as such in Europe. Ambulance
personnel in the first responding units are sometimes provided with extensive training,
which may be from 400 to 500 hours. In Oslo, for example, ambulance personnel (equivalent
to US basic EMTs) are taught to perform endotracheal intubation. In Holland a registered
nurse who can operate a manual defibrillator arrives on more than 80% of the
first-responding ambulances. Other systems, such as that in Göteborg, Sweden, use a
second responding unit manned by specially trained nurses on 24-hour duty, similar to a US
paramedic unit. Physician-manned mobile coronary care units are also common.
In other locations, especially in France, Israel, and Germany, and to a much lesser extent
in England, Australia,42 and Finland, emergency physicians (called ambulance doctors)
provide advanced cardiac life support.107 They respond in specially equipped vehicles, known as doctor-manned
ambulances. Systems in the United States, however, abandoned programs with physicians
or nurses on ambulances years ago because physician-staffed ambulances in the United
States were considered an inefficient use of physician resources. In addition, paramedics
can perform the same functions with comparable effectiveness.140
Physician-staffed ambulances in Europe, however, may well be more cost-effective than they
are in the United States, depending on relative operating costs, professional salaries,
population density, and combined services such as air rescue. In Norway, for example, nine
doctor-ambulance units combined with helicopter services respond effectively to about
4,500 patients a year in a population service area of 4 million people. These units depend
on public subscriptions and have been quite popular. In Australia several states and
localities use a single-layer ambulance response. The ambulance training, however,
includes both early defibrillation and administration of up to 20 drugs (but not
intubation). The guiding principle in all systems, no matter how organized, is to provide
the necessary treatment to the patient in the most timely and cost-effective manner.
|
| Table 3. Range of Rates of Survival to Hospital
Discharge for All Cardiac Arrest Rhythms and for Ventricular Fibrillation by System Type* |
|
| System type |
Survival: all
rhythms |
Weighted
average |
Survival: ventricular
fibrillation |
Weighted overages
for survival |
|
| EMT/AMB only |
2-9% |
5% |
3-20% |
12% |
| EMT/AMB-D |
4-19% |
10% |
6-26% |
16% |
| Paramedics/doctors only |
7-18% |
10% |
13-30% |
17% |
| EMT/AMB+paramedics/doctors |
4-26% |
17% |
23-33% |
26% |
| EMT/AMB-D+paramedics/doctors |
13-18% |
17% |
27-29% |
29% |
|
EMT/AMB, Basic emergency medical technicians or ambulance
personnel.31,33,77,78,88,90,122,142,152,153
EMT/AMB-D, Emergency medical technicians or ambulance personnel who are
trained to defibrillate.77,88,90,119,122
Paramedics/doctors only, Ambulance vehicles staffed with paramedics or
doctors.6,33-35,76-86
EMT/AMB+paramedics/doctors, Ambulance vehicles staffed with basic
emergency medical technicians or ambulance personnel plus second response vehicles staffed
with paramedics or doctors.33,38,39,101,154-158
EMT/AMB-D+paramedics/doctors, Ambulance vehicles staffed with emergency
medical technicians or ambulance personnel who are trained to defibrillate, plus second
response vehicles staffed with paramedics or doctors.89,143
*Data from 31 locations. |
Defibrillation and advanced cardiac life support.
Observers classically have considered defibrillation a part of advanced cardiac life
support care. Now, however, early defibrillation is a separate link in the chain of
survival. EMTs and other early responders113 share this skill with paramedics, physicians, and nurses. Still,
in view of the simultaneous therapies employed during a resuscitation attempt, it is
difficult to separate the value of defibrillation from the value of intubation and
intravenous medications.
What incremental benefit can be derived from these advanced procedures compared with
defibrillation alone? Evidence from different locations, with different emergency response
systems, sheds some light on this question. Differences in survival rates exist between a
system that provides only early defibrillation and early advanced cardiac care. These
differences may indicate the additional benefit of advanced cardiac life support. In Iowa,
for example, small communities that have provided early defibrillation without prehospital
advanced cardiac life support care have achieved a ventricular fibrillation survival rate
of 19%.90 Meanwhile, suburban King County, Washington, which uses a tiered
system (early defibrillation crews followed by advanced cardiac life support crews), has
achieved an even greater survival rate. This system reports a 29% survival rate for
patients with witnessed ventricular fibrillation arrest.89 Emergency
personnel resuscitated about 30% of persons who survived with defibrillatory shocks alone,
either from emergency medical technicians trained to defibrillate (EMT-Ds) or from
paramedics. These people did not require subsequent intubation or intravenous medications.141
The average survival rate for EMT-D-only systems has been 16%43,90,119,120,142
(see Table 3). This rate refers to patients in witnessed
cardiac arrest and in ventricular fibrillation. This is significantly lower than the
average ventricular fibrillation survival rate of 29% in combined EMT-D and paramedic
systems.89,143 Paramedic-only systems have an average survival rate of 17%,
almost exactly the same survival rate as EMT-D-only systems.33-35,76-86
Paramedic-only and EMT-D-only systems average the same survival rate for a specific
reason. In paramedic-only systems all advanced cardiac life support interventions
(defibrillation, intubation, and administration of medications) are performed, but
performed late. Only basic CPR and defibrillation are performed in EMT-D-only systems, but
these interventions are performed much earlier.
These observations confirm that a considerable portion of all survivors are alive because
of early defibrillation alone. These data also imply the important additional value of
intubation and intravenous medications. Researchers think that these interventions not
only promote return of spontaneous rhythm and circulation but also stabilize and maintain
patients during the immediate postresuscitation period. Ventricular fibrillation survival
rates in EMT-D-only systems (Table 3) can be compared with
survival rates of tiered EMT-D/paramedics systems. Such a system comparison hints at the
relative value of these two system types. The table shows that EMT-D systems alone
resuscitate about half of all potential ventricular fibrillation survivors.
Systems already staffed with paramedics or, as in Europe, with doctor-manned ambulances
should consider the addition of a basic EMT- or ambulance-defibrillation program, which
may significantly increase the ventricular fibrillation survival rate. However, no system
should delay the start of an early defibrillation program because of the absence of
paramedics or doctor-manned ambulances. In fact, some paramedic-only42 or doctor-manned
systems73,111 have such long response times and such poor outcomes that they may
be abandoned in favor of or supplemented by early automated defibrillation.
Resources may prevent establishment of a tiered response system that includes
first-responder defibrillation as well as paramedics. In these circumstances,
first-responder defibrillation, rather than paramedics alone, is probably the most
efficient method to improve survival from cardiac arrest. For locations without an
effective method of rapid delivery of prehospital defibrillation, the rational approach is
to start with first-responder automated defibrillation. Innovative leaders in such
locations as Japan,144 Scotland,25 Singapore,112 England,6 Norway,110 Australia,111,145 Sweden,43 and Hong Kong146 have all abandoned inappropriate plans to institute or continue
paramedic systems. Instead, these programs are going directly to the more efficient and
more effective approach of automated defibrillation.
Commentary
What is the maximum practical survival rate? The number of people resuscitated from sudden
cardiac death by emergency personnel is not known. Nor is it known how many people can be
resuscitated with a reasonable chance of surviving and remaining neurologically intact.
Cardiac disease, in general, is the single greatest cause of death in the United States.22,147 For
the adult American population, epidemiologists have estimated the annual incidence of
out-of-hospital sudden cardiac arrest at about 1 in 1,000 per year.147 Other statistics
from the American Heart Association are often quoted: 1.5 million "generic"
heart attacks per year in the United States, of which 25%, or 350,000-400,000, die out of
the hospital.147 Though no national averages are available on the proportion of
people who survive out-of-hospital cardiac arrests, current estimates suggest that no more
than 1-3% of victims live to be discharged from the hospital. The true percentage is
probably even less.148
It could be argued that the highest survival rates currently reported for out-of-hospital
cardiac arrests are a reasonable target for all locations. While achievements of such
survival rates are not practical in every community, this approach does expose the gap
between what a community does achieve and what is possible. The highest published rates
come from sophisticated urban/suburban systems like King County, Wisconsin,62 and
Seattle.143 Both can be described as mature EMS systems. Over the past 10-15
years these locations established strong links in the chain of survival. The annual
survival rates for King County, Washington, from 1976 through 1987, fluctuate between 15%
and 20% for all cardiac arrests and 25-30% for all patients in ventricular fibrillation (Figure 2). These overall survival rates, however, have remained
moderately stable despite a number of system interventions, such as EMT defibrillation
with manual defibrillators,88 EMT defibrillation with automated defibrillators,98
dispatcher-assisted CPR,51 and transcutaneous pacing.149 Therefore, this
level of ventricular fibrillation survival may represent the practical limits for
prehospital emergency care.
How many people would survive if all emergency medical systems in the United States
approached the hypothesized maximum survival rate of 20% that occurs in these mature EMS
systems? If an estimated 3% survival rate148 is applied to the presumed annual 400,000 cardiac arrests,
approximately 12,000 people per year now survive out-of-hospital cardiac arrest.147 A 20%
survival rate for this population of nontraumatic cardiac arrest patients would yield
80,000 survivors, or an additional 68,000 people. The American Heart Association estimates
that nationwide implementation of all life-saving emergency cardiac care mechanisms in
each community may save between 100,000 and 200,000 lives annually in the United States.1 Without
proper implementation of a full prehospital care system, however, emergency services
cannot achieve such rates. People not resuscitated before hospital arrival rarely survive.150,151
Figure 2. Ventricular fibrillation survival rates over
time. Percentage of people in nontraumatic cardiac arrest with initial rhythm ventricular
fibrillation who survive to hospital discharge. Data from King County, Washington,
Division of Emergency Medical Services, Seattle-King County Department of Public Health,
Seattle.
|
 |
Design Imitation?
Is it possible for EMS systems to imitate the design of more successful locations and thus
achieve the same survival rates? Table 3 summarizes data
published on cardiac arrest survival from many cities worldwide.31, 33-35, 38, 39, 43, 76-90, 101, 119, 120, 142, 143,
152-158. These data show marked variation in
survival rates among the different types of EMS systems, ranging from 5% to 17% survival
for patients in all cardiac arrest rhythms and from 12% to 29% for patients specifically
in ventricular fibrillation.
Simple structural imitation of successful EMS organizations, however, does not always
succeed. Even in locations with similarly structured EMS systems, marked differences in
the observed survival rates persist. For example, studies from 15 different paramedic-only
or doctor-manned ambulance systems (Table 3, row C) reported
survival rates from 7% to 18% for all rhythms and from 13% to 30% for ventricular
fibrillation.6,33-35,76-86 Table 3 summarizes results from nine
EMT-paramedic systems (row D). These systems display the same wide variations.33,38,39,101,154-158
It is unclear exactly why these differences occur within the same types of systems. Part
of the explanation is that definition of terms and reporting of data are not standardized.159 While
some researchers have proposed uniform reporting systems, many others have pointed to the
need for an international standardized nomenclature.18,27,35,39,87,159,160 Regardless, part of these differences may very well be due to
variable effectiveness or lack of EMS medical leadership and direction.161-165
It can also be argued that similarly constructed systems have different survival rates
because they differ in how well they develop and implement each link in the chain of
survival.87,163,166 This appears particularly true for early initiation of CPR and
early arrival of personnel trained to operate a defibrillator. Many cities in the United
States, for example, established a strong link for early advanced life support by starting
paramedic services at great expense and effort.33-35,76-86 Most of
these paramedic-only systems have achieved disappointingly low survival rates. In part
this is because citizens in these locations seldom attempted to perform CPR. In addition,
long paramedic response times, in the absence of an early defibrillation program,
precluded early defibrillation and early advanced care. In paramedic-only systems,
paramedics are generally preoccupied with many other minor emergencies and consequently
are less available (and less skilled) to deal with cardiac arrest patients.163
To strengthen the early CPR link in the chain of survival, several EMS systems have
mounted extensive CPR campaigns. They have trained a large percentage of the population in
basic CPR skills. Unfortunately, these systems also have observed diminished survival
rates because they failed to provide an emergency medical service with rapid
defibrillation and rapid advanced life support.18,39,43,78,153,155
Enhancements of early CPR programs, such as targeted CPR training10,53-59 and
dispatcher-assisted CPR programs,51,65,67 will also fail if defibrillation does not occur soon after
collapse.
Conversely, systems that have established early defibrillation programs by training their
less advanced ambulance personnel to use defibrillators43,90,119,120,142
may experience low success rates if they do not also train citizens to recognize cardiac
arrest early or to call the emergency service immediately. The defibrillator will not
arrive quickly enough if the EMS system is not called immediately, if local ambulances or
first-responder units are not equipped with defibrillators, or if managers do not
strategically deploy emergency response vehicles with defibrillators.
Responsible people must apply continuous quality improvement concepts to each link in the
chain of survival. In early CPR, for example, it is not only a matter of the number of
people who are trained. Systems can achieve better results by targeting the right groups
and evaluating training programs, short-term results, and long-term trends. Automated
defibrillators must be placed, then complemented with carefully planned training and
follow-up programs and close medical control of the system, including individual case
reviews and overall data management programs. Without these quality improvement methods, a
system will not realize the full benefit of any new organization.
Summary
The chain of survival concept embodies standard principles of system management. The
phrase restates167 the familiar emergency medical services continuum pioneered by
Peter Safar, who coined the term life support chain.168 Other authors
have referred to the concept with various phrases.1,3,20,23,140 As a
pedagogic construct, it emphasizes that there are no easy, single-step approaches to
improving survival from cardiac arrest.166,167
Early access to the EMS system ensures early CPR, defibrillation, and advanced care. Early
access is easiest to achieve with 911 systems and widespread community education and
publicity. Instructors may also teach early access during citizen CPR classes. Early CPR
helps patients by slowing the process of dying, but its effectiveness disappears within
minutes, and defibrillation must soon follow. Early recognition and early CPR are best
achieved when citizens are well informed about cardiac emergencies and well trained in
CPR. The earliest possible delivery of defibrillation is critical and almost by itself is
sufficient for many victims of sudden cardiac death.
Defibrillation has therefore emerged as the single most effective intervention for
patients in nontraumatic cardiac arrest. Automated external defibrillators help to
accomplish this goal and permit widespread implementation of a variety of early
defibrillation programs. Early advanced care helps those who do not immediately convert to
an organized cardiac activity or who do not achieve a spontaneous circulation following
early defibrillation. Advanced care allows the highest possible survival rate through
respiratory and antiarrhythmic stabilization and monitoring of patients in the
post-resuscitation period.
At present, early CPR and rapid defibrillation, combined with early advanced care, can
result in long-term survival rates for witnessed ventricular fibrillation as high as 30%.
Researchers have observed that neurological and psychological recovery from cardiac arrest
depends on the time within which these critical interdependent treatment modalities are
delivered.22,169 Therefore, high resuscitation rates will also lead to a high
percentage of patients who recover to the neurological level they had before their arrest.
The future of the chain of survival will be highly dependent on multicenter cooperative
studies of cardiac arrest in both in-hospital and out-of-hospital settings.150,162,170
In addition to scientific research, the training of those responsible for implementing and
maintaining the chain of survival must become a priority.150,162,164 For
emergency medical services the challenge is to develop programs that will allow
recognition, access, bystander CPR, defibrillation, and advanced care to occur as quickly
as possible. Ideally systems should deliver these interventions within moments after
sudden death victims collapse. Achievement of such a goal requires the deployment of
multiple, properly directed programs, within an EMS system. Each program should lend
strength to the chain of survival, thereby enhancing successful recovery and long-term
survival.
Recommendations
The Advanced Cardiac Life Support Subcommittee and the Emergency Cardiac Care Committee of
the American Heart Association recommend that all communities take the following actions
to strengthen their Chain of Survival:
1. Early Access
- All communities should implement an enhanced 999 system.
- All communities should develop education and publicity
programs that focus on cardiac emergencies and a proper response by citizens.
2. Early CPR
- Communities should continue to vigorously implement and
support community-wide CPR training programs.
- Community CPR programs should emphasize early recognition,
early telephone contact with the EMS system, and early defibrillation.
- Community CPR programs should develop and use training
methods that will increase the likelihood that citizens will actually initiate CPR.
- Communities should adopt more widespread and effective
targeted CPR programs.
- Communities should implement programs to establish
dispatcher-assisted CPR.
3. Early Defibrillation
- All communities should adopt the principle of early
defibrillation. This principle applies to all personnel who are expected, as part of their
professional duties, to perform basic CPR: they must carry an automated external
defibrillator and be trained to operate it.
- Health professionals who have a duty to respond to a person
in cardiac arrest should have a defibrillator available either immediately or within 1-2
minutes.
- Responsible personnel should authorize and implement more
widespread use of automated external defibrillation by community responders and allied
health responders.
4. Early Advanced Life Support
- Advanced life support units should be combined with
first-responding units that provide early defibrillation.
- Advanced life support units should develop well-coordinated
protocols that combine rapid defibrillation by first-responding units with rapid
intubation and intravenous medications by the advanced cardiac life support units.
Acknowledgments
Over the years many people have contributed to the chain of survival concept. In
particular, we want to mention Professor F. W. Ahnefeld of Ulm, Germany, who pioneered the
"rescue chain" concept in emergency medical care in the early 1960s.
The Advanced Cardiac Life Support Subcommittee and the Emergency Cardiac Care Committee
thank the following persons for their contributions to this statement: Mickey Eisenberg,
Tore Laerdal, Leo Bossaert, Stig Holmberg, Thomas R. Hearne, Judith Reid Graves, Allan
Jaffe, Mary Newman, Mary Pat Larsen, and Douglas Austin Jr.
References
1. Standards and guidelines for cardiopulmonary
resuscitation (CPR) and emergency cardiac care (ECC). JAMA 1986;255:2905-2914
2. Graf WS, Polin SS, Paegel BL: A community program for
emergency cardiac care: A three-year coronary ambulance-paramedic evaluation. JAMA 1973;226:156-160
3. Schwartz L: Pre-hospital care: Field intervention
medicine, in Schwartz GR, Safar P, Stone J, Storey P, Wagner D (eds): Principles and
Practice of Emergency Medicine. Philadelphia, WB Saunders Co, 1986, pp 593-619
4. Hallstrom AP; Improving the EMS system, in Eisenberg
MS, Bergner L, Hallstrom AP (eds): Sudden Cardiac Death in the Community, Philadelphia,
Praeger Pubs, 1984, pp 126-139
5. American Red Cross: Adult CPR. Boston, Mass,
American National Red Cross, 1987
6. Walters G. Glucksman E: Planning a pre-hospital cardiac
resuscitation programme: An analysis of community and system factors in London. J R
Coll Physicians Lond 1989;23:107-110
7. Stults KR: Phone first. J Emerg Med Services 1987;12:28
8. Hunt RC, Allison EJ Jr, Yates JG III: The need for
improved emergency medical services in Pitt county. N C Med J 1986;47:39-42
9. Hunt RC, McCabe JB, Hamilton GC, Krohmer JR: Influence
of Emergency Medical Services systems and prehospital defibrillation on survival of sudden
cardiac death victims. Am J Emerg Med 1989;7:68-82
10. Mandel LP, Cobb LA: CPR training in the community. Ann
Emerg Med 1985;14:669-671
11. Mayron R, Long RS, Ruiz E: The 911 emergency telephone
number: Impact on emergency medical systems access in a metropolitan area. AM J Emerg
Med 1984;2:491-493
12. Eisenberg M, Hallstrom A, Becker L: Community
awareness of emergency phone numbers. Am J Public Health 1981;71:1058-1060
13. Cummins RO, Eisenberg MS: Prehospital cardiopulmonary
resuscitation: Is it effective? JAMA 1985;253:2408-2412
14. Thompson BM, Stueven HA, Mateer JR, Aprahamian CC,
Tucker JF, Darin JC: Comparison of clinical CPR studies in Milwaukee and elsewhere in the
United States. Ann Emerg med 1985;14:750-754
15. Kowalski R, Thompson BM, Horwitz L, Stueven H,
Aprahamian C, Darin JC: Bystander CPR in prehospital coarse ventricular fibrillation. Ann
Emerg Med 1984;13:1016-1020
16. Kouwenhoven WB, Jude JR, Knickerbocker GG:
Closed-chest cardiac massage. JAMA 1960;173:1064-1067
17. Safar P, Brown TC, Holtey WJ, Wilder RJ: Ventilation
and circulation with closed-chest cardiac massage in man. JAMA 1961;176:574-576
18. Bossaert L, Van Hoeyweghen R, Cerebral Resuscitation
Study Group: Bystander cardiopulmonary resuscitation (CPR) in out-of-hospital cardiac
arrest. Resuscitation 1989;17(suppl):S55-S69
19. Cummins R, Graves J: Clinical results of standard CPR:
Prehospital and inhospital, in Kaye W, Bircher N (eds): Cardiopulmonary Resuscitation. New
York, Churchill Livingstone, Inc., 1989, pp 87-102
20. Advanced cardiac life support in perspective, in Textbook
of Advanced Cardiac Life Support. Dallas, American Heart Association, 1987, pp 1-10
21. Safar P: History of cardiopulmonary-cerebral
resuscitation, in Kaye W, Bircher N (eds): Cardiopulmonary Resuscitation. New York,
Churchill Livingstone, Inc, 1989, pp 1-54
22. Pepe P: Advanced cardiac life support: State of the
art, in Vincent JL (ed): Emergency and Intensive Care. Berlin, Springer-Verlag,
1990, pp 565-585
23. Putting it all together: Resuscitation of the patient,
in Textbook of Advanced Cardiac Life Support. Dallas, American Heart Association,
1987, pp 235-248
24. Eisenberg M, Bergner L, Hallstrom A: Paramedic
programs and out-of-hospital cardiac arrest: I. Factors associated with successful
resuscitation. Am J Public Health 1979;69:30-38
25. Carrington D: Heartstart Scotland: Early
defibrillation for the whole of Scotland, in Proceedings of the 6th World Congress on
Disaster and Emergency Medicine. Hong Kong, Excerpta Medica, 1989, p 66
26. Pepe P: Presumptive diagnosis of death versus whom to
resuscitate, in Kuehl A (ed): EMS Medical Director’s Handbook for the National
Association of EMS Physicians. St. Louis, CV Mosby Co, 1989, pp 275-289
27. Mullie A, Van Hoeyweghen R, Quets A, Cerebral
Resuscitation Study Group: Influence of time intervals on outcome of CPR. Resuscitation
1989;17(suppl):S23-S33
28. Lund I, Skulberg A: Cardiopulmonary resuscitation by
lay people. Lancet 1976;2:702-704
29. Copley DP, Mantle JA, Rogers WJ, Russell RO Jr:
Improved outcome for prehospital cardiopulmonary collapse with resuscitation by
bystanders. Circulation 1977;56:901-905
30. Thompson RG, Hallstrom AP, Cobb LA:
Bystander-initiated cardiopulmonary resuscitation in the management of ventricular
fibrillation. Ann Intern Med 1979;90:737-740
31. Tweed WA, Bristow G, Donen N: Resuscitation from
cardiac arrest: Assessment of a system providing only basic life support outside of
hospital. Can Med Assoc J 1980;122:297-300
32. Gudjonsson H, Baldvinsson E, Oddsson G, Asgeirsson E,
Kristjansson H, Hardarson T: Results of attempted cardiopulmonary resuscitation of
patients dying suddenly outside the hospital in Reykjavik and the surrounding area,
1976-1979. Acta Med Scand 1982;212:247-251
33. Vertesi L, Wilson L, Glick N: Cardiac arrest:
Comparison of paramedic and conventional ambulance services. Can Med Assoc J 1983;128:809-812
34. Guzy PM, Pearce ML, Greenfield S: The survival benefit
of bystander cardiopulmonary resuscitation in a paramedic-served metropolitan area. Am
J Public Health 1983;73:766-769
35. Roth R, Stewart RD, Rogers K, Cannon GM:
Out-of-hospital cardiac arrest: Factors associated with survival. Ann Emerg Med 1984;13:237-243
36. Stueven H, Troiano P, Thompson B, Mateer JR, Kastenson
EH: Bystander/first responder CPR: Ten years experience in a paramedic system. Ann
Emerg Med 1986;15:707-710
37. Ritter G, Wolfe RA, Goldstein S, Landis JR, Vasu CM,
Acheson A, Leighton R, Medendrop SV: The effect of bystander CPR on survival of
out-of-hospital cardiac arrest victims. Am Heart J 1985;110:932-937
38. Cummins RO, Eisenberg MS, Hallstrom AP, Litwin PE:
Survival of out-of-hospital cardiac arrest with early initiation of cardiopulmonary
resuscitation. Am J Emerg Med 1985;3:114-119
39. Eitel DR, Walton SL, Guerci AD, Hess DR, Sabulsky NK:
Out-of-hospital cardiac arrest: A six-year experience in a suburban-rural system. Ann
Emerg Med 1988;17:808-812
40. Spaite DW, Hanlon T, Criss EA, Valenzuela TD, Wright
AL, Keeley KT, Meislin HW: Prehospital cardiac arrest: The impact of witnessed collapse
and bystander CPR in a metropolitan EMS system with short response times. Ann Emerg Med
1990;19:1264-1269
41. Lewi PJ, Mullie A, Quets A: Relevance and significance
of pre-CPR conditions in cardiopulmonary-cerebral resuscitation: A graphic analysis by
means of Spectramap. Resuscitation 1989;17(suppl):S35-S44
42. Wright D, James C, Marsden AK, Mackintosh AF:
Defibrillation by ambulance staff who have had extended training. BMJ 1989;299:96-97
43. Jakobsson J, Nyquist O, Rehnqvist N: Cardiac arrest in
Stockholm with special reference to the ambulance organization. Acta Med Scand 1987;222:117-122
44. Weaver WD, Cobb LA, Dennis D, Ray R, Hallstrom AP,
Copass MK: Amplitude of ventricular fibrillation waveform and outcome after cardiac
arrest. Ann Intern Med 1985;102:53-55
45. Selby ML, Kautz JA, Moore TJ, Gombeski WR Jr, Ramirez
AG, Farge EJ, Forthofer RN: Indicators of response to a mass media CPR recruitment
campaign. Am J Public Health 1982;72:1039-1042
46. St. Louis P, Carter WB, Eisenberg MS: Prescribing CPR:
A survey of physicians. Am J Public Health 1982;72:1158-1160
47. Goldberg RJ: Physicians and CPR training in high-risk
family members. Am J Public Health 1987;77:671-672
48. Cobb LA, Werner JA, Trobaugh GB: Sudden cardiac death:
I. A decade’s experience with out-of-hospital resuscitation. Mod Concepts
Cardiovasc Dis 1980;49:31-36
49. Murphy RJ, Luepker RV, Jacobs DR Jr, Gillum RF, Folsom
AR, Blackburn H: Citizen cardiopulmonary resuscitation training and use in a metropolitan
area; The Minnesota Heart Survey. Am J Public Health 1984;74:513-515
50. Gombeski WR Jr, Effron DM, Ramirez AG, Moore TJ:
Impact on retention: Comparison of two CPR training programs. Am J Public Health 1985;72:849-852
51. Eisenberg MS, Hallstrom AP, Carter WB, Cummins RO,
Bergner L, Pierce J: Emergency CPR instruction via telephone. Am J Public Health 1985;75:47-50
52. McCormack AP, Damon SK, Eisenberg MS: Disagreeable
physical characteristics affecting bystander CPR. Ann Emerg Med 1989;18:283-285
53. Cobb LA, Hallstrom AP, Thompson RG, Mandel LP, Copass
MK: Community cardiopulmonary resuscitation. Annu Rev Med 1980;31:453-462
54. Cobb LA, Hallstrom AP: Community-based cardiopulmonary
resuscitation: What have we learned? Ann N Y Acad Sci 1982;382:330-342
55. Bossaert L, Van Hoeyweghen R, Cerebral Resuscitation
Study Group: Evaluation of cardiopulmonary resuscitation (CPR) techniques. Resuscitation
1989;17(suppl):S99-S109
56. Murphy RJ, Luepker RV, Jacobs DR Jr, Gillum RF, Folsom
AR, Blackburn H: Citizen cardiopulmonary resuscitation training and use in a metropolitan
area: The Minnesota Heart Survey. Am J Public Health 1984;74:513-515
57. Goldberg RJ, Gore JM, Love DG, Ockene JK, Dalen JE:
Layperson CPR – Are we training the right people? Ann Emerg Med 1984;13:701-704
58. Pane G, Salness K: Targeted recruitment of senior
citizens and cardiac patients to a mass CPR training course. Ann Emerg Med 1989;18:152-154
59. Pane GA, Salness KA: A survey of participants in a
mass CPR training course. Ann Emerg Med 1987;16:1112-1116
60. Litwin PE, Eisenberg MS, Hallstrom AP, Cummins RO: The
location of collapse and its effect on survival from cardiac arrest. Ann Emerg Med 1987;16:787-791
61. Kraus JF, Borhani NO, Franti CE: Socioeconomic status,
ethnicity and risk of coronary heart disease. Am J Epidemiol 1980;111:407-414
62. Eisenberg MS: Who shall live? Who shall die? in
Eisenberg MS, Bergner L, Hallstrom AP (eds): Sudden Cardiac Death in the Community. Philadelphia,
Praeger Pubs, 1984, pp 44-58
63. Bonnin M, Pepe P, Clack P: Survival prognosis for the
elderly after out-of-hospital cardiac arrest (abstract). Ann Emerg Med 1989;18:469
64. Safar P, Abramson N, Detre K: Old age does not negate
good outcome after cardiac arrest and CPR (abstract). Crit Care Med 1989;17:575
65. Carter WB, Eisenberg MS, Hallstrom AP, Schaeffer S:
Development and implementation of emergency CPR instructions via telephone. Ann Emerg
Med 1984;13:695-700
66. Clawson JJ: Emergency medical dispatching, in Roush
WR, Aranosian RD, Blair TMH, Handal KA, Kellow RD, Stewart RD (eds): Principles of EMS
Systems: A Comprehensive Text for Physicians. Dallas, American College of Emergency
Physicians, 1989, pp 119-133
67. Kellerman AL, Hackman BB, Somes G: Dispatcher-assisted
cardiopulmonary resuscitation: Validation of efficacy. Circulation 1989;80:1231-1239
68. Bayés de Luna A, Coumel P, Leclercq JF: Ambulatory
sudden cardiac death: Mechanisms of production of fatal arrhythmia on the basis of data
from 157 cases. Am Heart J 1989;117:151-159
69. Fletcher GF, Cantwell JD: Ventricular fibrillation in
a medically supervised cardiac exercise program: Clinical, angiographic, and surgical
correlations. JAMA 1977;238:2627-2629
70. Haskell WL: Cardiovascular complications during
exercise training of cardiac patients. Circulation 1978;57:920-924
71. Hossack KF, Hartwig R: Cardiac arrest associated with
supervised cardiac rehabilitation. J Cardiac Rehab 1982;2:402-408
72. Van Camp SP, Peterson RA: Cardiovascular complications
of outpatient cardiac rehabilitation programs. JAMA 1986;256:1160-1163
73. Colquhoun MC: Use of defibrillators by general
practitioners. BMJ 1988;297:336-337
74. Rawlins DC: Study of the management of suspected
cardiac infarction by British immediate care doctors. Br Med J [Clin Res] 1981;282:1677-1697
75. Pai GR, Haites NE, Rawles JM: One thousand heart
attacks in Grampian: The place of cardiopulmonary resuscitation in general practice. Br
Med J [Clin Res] 1987;294:352-354
76. Amey BD, Harrison EE, Straub EJ: Sudden cardiac death:
A retrospective and prospective study. JACEP 1976;5:429-433
77. Bachman JW, McDonald GS, O’Brien PC; A study of
out-of-hospital cardiac arrests in northeastern Minnesota. JAMA 1986;256:477-483
78. Crawford GC, Denton M, Fisher CA, Giaonz IL, Sharpe N,
Scragg R: Resuscitation outside hospital in Auckland, N Z Med J 1986;99:452-455
79. Diamond NJ, Schofferman J, Elliott JW: Factors in
successful resuscitation by paramedics. JACEP 1977;6:42-46
80. Eisenberg MS, Hadas E, Nuri I, Applebaum D, Roth A,
Litwin PE, Hallstrom A, Nagel E: Sudden cardiac arrest in Israel: Factors associated with
successful resuscitation. Am J Emerg Med 1988;6:319-323
81. Goldstein S, Landis JR, Leighton R, Ritter G, Vasu CM,
Lantis A, Serokman R: Characteristics of the resuscitated out-of-hospital cardiac arrest
victim with coronary heart disease. Circulation 1981;64:977-984
82. Lauterbach SA, Spadafora M, Levy R: Evaluation of
cardiac arrest managed by paramedics. J Am Coll Emerg Med 1978;7:355-357
83. Liberthson RR, Nagel EL, Hirschman JC, Nussenfeld JD:
Prehospital ventricular defibrillation: Prognosis and follow-up course. N Engl J Med 1974;291:317-321
84. Mackintosh AF, Crabb ME, Grainger R, Williams JH,
Chamberlain DA: The Brighton resuscitation ambulances: Review of 40 consecutive survivors
of out-of-hospital cardiac arrest. Br Med J [Clin Res] 1978;1:1115-1118
85. McSwain GR, Garrison WB, Artz CP: Evaluation of
resuscitation from cardiopulmonary arrest by paramedics. Ann Emerg Med 1980;9:341-345
86. Rose LB: The Oregon Coronary Ambulance Project: An
experiment. Heart Lung 1974;3:753-755
87. Eisenberg MS, Horwood BT, Cummins RO, Reynolds-Haertle
R. Hearne TR: Cardiac arrest and resuscitation: A tale of 29 cities. Ann Emerg Med 1990;19:179-186
88. Eisenberg MS, Copass MK, Hallstrom AP, et al:
Treatment of out-of-hospital cardiac arrest with rapid defibrillation by emergency medical
technicians N Engl J Med 1980;302:1379-1383
89. Eisenberg MS, Hallstrom AP, Copass MK, Bergner L,
Short F, Pierce J: Treatment of ventricular fibrillation: Emergency medical technician
defibrillation and paramedic services. JAMA 1984;251:1723-1726
90. Stults KR, Brown DD, Schug VL, Bean JA: Prehospital
defibrillation performed by emergency medical technicians in rural communities. N Engl
J Med 1984;310:219-223
91. Weaver WD, Copass MK, Bufi D, Ray R, Hallstrom AP,
Cobb LA: Improved neurologic recovery and survival after early defibrillation. Circulation
1984;69:943-948
92. White RD: EMT-defibrillation: Time for controlled
implementation of effective treatment. Emerg Cardiac Care Newsletter 1986;8:1-3
93. Cummins RO: EMT-defibrillation: National guidelines
for implementation. Am J Emerg Med 1987;5:254-257
94. Cummins RO, Eisenberg MS, Moore JE, Hearne TR,
Andresen E, Wendt R, Litwin PE, Graves JR, Hallstrom AP, Pierce J: Automatic external
defibrillators: Clinical, training, psychological, and public health issues. Ann Emerg
Med 1985;14:755-760
95. Cummins RO: From concept to standard-of-care? Review
of the clinical experience with automated external defibrillators. Ann Emerg Med 1989;18:1269-1275
96. Cummins RO, Eisenberg MS, Bergner L, Hallstrom AP,
Hearne T, Murray JA: Automatic external defibrillation: Evaluations of its role in the
home and in emergency medical services. Ann Emerg Med 1984;13(9, pt 2):789-801
97. Cummins RO, Eisenberg MS, Stults KR, Automatic
external defibrillators: Clinical issues for cardiology. Circulation 1986;73:381-385
98. Cummins RO, Eisenberg MS, Litwin PE, Graves JR, Hearne
TR, Hallstrom AP: Automatic external defibrillators used by emergency medical technicians:
A controlled clinical trail. JAMA 1987;257:1605-1610
99. Stults KR, Brown DD, Kerber RE: Efficacy of an
automated external defibrillator in the management of out-of-hospital cardiac arrest;
Validation of the diagnostic algorithm and initial experience in a rural environment. Circulation
1986;73:701-709
100. Paris PM: EMT-defibrillation: A recipe for saving
lives. Am J Emerg Med 1988;6:282-287
101. Weaver WD, Cobb LA, Hallstrom AP, Copass MK, Ray R,
Emery M, Fahrenbruch C: Considerations for improving survival from out-of-hospital cardiac
arrest. Ann Emerg Med 1986;15:1181-1186
102. Atkins J, Streigler H, Burstain T, Foster G: Improved
survival rates with automatic defibrillators (abstract). Prehospital Disaster Med 1989;1:69
103. Cummins RO, Stults KR, Haggar B, Kerber RE, Schaeffer
S, Brown DD: A new rhythm library for testing automatic external defibrillators:
Performance of three devices. J Am Coll Cardiol 1988;11:597-602
104. Bocka JJ: Automatic external defibrillators. Ann
Emerg Med 1989;18:1264-1268
105. Edwards DG: Development of a decision algorithm for a
semiautomatic defibrillator. Ann Emerg Med 1989;18:1276-1279
106. Stults KR, Cummins RO: Fully automatic vs. shock
advisory defibrillators: What are the issues? J Emerg Med Services 1987;71-73
107. Newman MM: Advancing resuscitation abroad. J Emerg
Med Services 1987;12:22-26
108. Newman MM: An international movement for earlier
defibrillation. J Emerg Med Services 1988;13:19-21
109. Fonsmark L, Sandře E, Kastrup J, Svendsen JH:
Treatment of cardiac arrest outside of the hospital with a semiautomatic defibrillator
– Heartstart 2000. Ugeskr Laeger 1989;151:1048-1051
110. Hapnes S: The chain of survival: The Scandinavian
experience, in Proceedings of the 6th World Congress on Disaster and Emergency
Medicine. Hong Kong, Excerpta Medica, 1989, p 43
111. Bett JH: Experience with a mobile coronary care unit
in Brisbane. Ann Emerg Med 1989;18:969-974
112. Anatharaman V, Koo C, Tan T: Pre-hospital cardiac
defibrillation programme in Singapore, in Proceedings of the 6th World Congress on
Disaster and Emergency Medicine. Hong Kong, Excerpta Medica, 1989, p 44
113. Newman MM: Defibrillation shakes the nation: Results
of the Journal of Emergency Medical Services 1988 National Early Defibrillation Study. J
Emerg Med Services 1989;14:50-59
114. Newman MM: The survival advantage: Early
defibrillation programs in the fire service. J Emerg Med Services 1987;12:40-46
115. Murphy DM: Rapid defibrillation: Fire service to lead
the way. J Emerg Med Services 1987;12:67-71
116. Murphy DM: RapidZap, in Graves JR, Austin DJ, Cummins
RO (eds): RapidZap: Automatic Defibrillation. Englewood Cliffs, NJ, Brady
Communications Co, Inc, 1989, pp 1-3
117. IAFC on Scene, Newsletter, International
Association of Fire Chiefs. Washington, DC, 1987, p 1
118. Dibbs E, Thomas HE Jr, Weiss ST, Sparrow D: Fire
fighting and coronary heart disease. Circulation 1982;65:943-946
119. Vukov LF, White RD, Bachman JW, O’Brien PC: New
perspective on rural EMT defibrillation. Ann Emerg Med 1988;17:318-321
120. Gray AJ, Redmond AD, Martin MA: Use of the automatic
external defibrillator-pacemaker by ambulance personnel: The Stockport experience. Br
Med J [Clin Res] 1987;294:1133-1135
121. Gentile D, Auerbach P, Gaffron J, Foon G, Phillips J
Jr: Prehospital defibrillation by emergency medical technicians: Results of a pilot study
in Tennessee. J Tenn Med Assoc 1988;81:144-148
122. Olson DW, LaRochelle J, Fark D, Aprahamian C,
Aufderheide TP, Mateer JR, Hargarten KM, Stueven HA: EMT-defibrillation: The Wisconsin
experience. Ann Emerg Med 1989;18:806-811
123. Jacobs L: Medical, legal, and social implications of
automatic external defibrillators. Ann Emerg Med 1986;15:863-864
124. Hallstrom AP, Eisenberg MS, Bergner L: The potential
use of automatic defibrillators in the home for management of cardiac arrest. Med Care 1984;22:1083-1087
125. Eisenberg MS, Cummins RO: Automatic external
defibrillation: Bringing it home. Am J Emerg Med 1984;3:568-569
126. Moore JE, Eisenberg MS, Cummins RO, Hallstrom A,
Litwin P, Carter W: Lay person use of automatic external defibrillation. Ann Emerg Med 1987;16:669-672
127. McDaniel CM, Berry VA, Haines DE, DiMarco JP:
Automatic external defibrillation of patients after myocardial infarction by family
members: Practical aspects and psychological impact of training. PACE 1988;11:2029-2034
128. Cummins RO, Schubach JA, Litwin PE, Hearne TR:
Training lay persons to use automatic external defibrillators: Success of initial training
and one-year retention of skills. Am J Emerg Med 1989;7:143-149
129. Chadda KD, Kammerer R: Early experiences with the
portable automatic external defibrillator in the home and public places. Am J Cardiol 1987;60:732-733
130. Chadda KD, Kammerer RJ, Kuphal J, Miller K:
Successful defibrillation in the industrial, recreational and corporate settings by
laypersons (abstract). Circulation 1987;76(suppl IV):IV-12
131. Swenson RD, Hill DL, Martin JS, Wirkus M, Weaver WD:
Automatic external defibrillators used by family members to treat cardiac arrest
(abstract). Circulation 1987;76(suppl IV):IV-463
132. Eisenberg MS, Moore J, Cummins RO, Andresen E, Litwin
PE, Hallstrom AP, Hearne T: Use of the automatic external defibrillator in home or
survivors of out-of-hospital ventricular fibrillation. Am J Cardiol 1989;63:443-446
133. Weaver WD, Sutherland K, Wirkus MJ, Bachman R:
Emergency medical care requirements for large public assemblies and a new strategy for
managing cardiac arrest in this setting. Ann Emerg Med 1989;18:155-160
134. Chapman PJC, Chamberlain DA: Death in the clouds. Br
Med J [Clin Res] 1987;294:181
135. Gessman LJ, Li JK-J, Lewandowski J, Yamazaki H,
Helfant RH: Transtelephonic resuscitation: A new approach to sudden death (abstract). Am
J Cardiol 1979;43:422
136. Ruffy R, Gessman LJ, Barbey JT, Allen ET, Smith M,
Steinberg S: Pilot study of transtelephonic cardioversion/defibrillation in man. Circulation
1987;76(suppl IV):IV-463
137. Dalzell GW, Cunningham SR, Prouzina S, Anderson J,
Magee H, Adgey AA: Assessment of a device for transtelephonic control of defibrillation. Lancet
1988;1:695-697
138. Herlitz B, Lebow F: Telephonic defibrillator helps
close "critical window." Emergency Medical News 1989;26:29
139. Associated Press: Portable defibrillator saves woman
stricken at home. Seattle Times, July 7, 1989, B-3
140. Atkins JM: Emergency medical service systems in acute
cardiac care: State of the art. Circulation 1986;74(suppl IV)IV-4-IV-8
141. Cummins RO, Graves JR, Horan S, Larsen MP, Crump K:
The relative contributions of early defibrillation and ACLS interventions to resuscitation
and survival from prehospital cardiac arrest (abstract). Ann Emerg Med 1989;18:468-469
142. Eisenberg MS, Bergner L, Hallstrom A: Out-of-hospital
cardiac arrest: Improved survival with paramedic services. Lancet 1980;1:812-815
143. Weaver WD, Hill D, Fahrenbruch CE, Copass MK, Martin
JS, Cobb LA, Hallstrom AP: Use of the automatic external defibrillator in the management
of out-of-hospital cardiac arrest. N Engl J Med 1988;319:661-666
144. Ishida T: Prognosis of cardiac arrest patients and
proposals for improved outcomes, in Proceedings of the 6th World Congress on
Disaster and Emergency Medicine. Hong Kong, Excerpta Medica, 1989, p 43
145. Oxer H: Strengthening the chain of survival:
Australia, in Proceedings of the 6th World Congress on Disaster and Emergency Medicine.
Hong Kong, Excerpta Medica, 1989, p 44
146. Moles M: Travel light, travel fast: Motorcycle
paramedics in Hong King. Prehospital Disaster Med 1989;4:179
147. 1987 Heart Facts. Dallas, American Heart
Association, 1986, p 31
148. Eisenberg MS, Bergner L, Halltsrom AP, Cummins RO:
Sudden cardiac death. Sci Am 1986;254:37-43
149. Cummins RO, Graves JR: Prehospital transcutaneous
pacing by paramedics and emergency medical technicians: Clinical and system effectiveness.
Prehospital Disaster Med 1989;4:196
150. Bonnin M, Pepe P: Key role of prehospital
resuscitation in survival from out-of-hospital cardiac arrest (abstract). Ann Emerg Med
1990;19:466
151. Kellermann AL, Staves DR, Hackman BB: In-hospital
resuscitation following unsuccessful prehospital advanced cardiac life support:
"Heroic efforts" or an exercise in futility? Ann Emerg Med 1988;17:589-594
152. Wilson BH, Severance HW Jr, Raney MP, Pressley JC,
McKinnis RA, Hindman MC, Smith M, Wagner GS: Out-of hospital management of cardiac arrest
by basic emergency medical technicians. Am J Cardiol 1984;53:68-70
153. Holmberg S, Wennerblom B: Out-of-hospital cardiac
arrest: Effect of special ambulances I Göteborg on mortality. Am J Emerg Med 1984;2:222-224
154. Lewis RP, Stang JM, Warren JV: The role of paramedics
in resuscitation of patients with prehospital cardiac arrest from coronary artery disease.
Am J Emerg Med 1984;2:200-203
155. Pressley JC, Raney MP, Wilson BH, Severance HW,
Wagner GS: Assessment of out-of-hospital resuscitation. Am J Emerg Med 1984;2:215-216
156. Stueven H, Troianop P, Thompson B, Mateer JR,
Kastenson EH, Tonsfeldt D, Hargarten K, Kowalski R, Aprahamian C, Darin J: Bystander/first
responder CPR: Ten years experience in a paramedic system. Ann Emerg Med 1986;15:707-710
157. Rockswold G, Sharma B, Ruiz E, Asinger R, Hodges M,
Brieter M: Follow-up of 514 consecutive patients with cardiopulmonary arrest outside the
hospital. JACEP 1979;8:216-220
158. Sammel NL, Taylor K, Selig M, O’Rourke MF: New
South Wales intensive care ambulance system: Outcome of patients with ventricular
fibrillation. Med J Aust 1981;2:546-550
159. Eisenberg MS, Cummins RO, Damon S, Larsen MP, Hearne
TR: Survival rates from out-of-hospital cardiac arrest: Recommendations for uniform
definitions and data to report. Ann Emerg Med 1990;19:1249-1259
160. Eisenberg MS, Bergner L, Hearne T: Out-of-hospital
cardiac arrest: A review of major studies and a proposed uniform reporting system. Am J
Public Health 1980;70:236-240
161. Pepe P: The past, present and future of emergency
medical services. Prehospital Disaster Med 1989;4:47-49
162. Pepe P, Bonnin M, Mattox K: Regulating the scope of
EMS. Prehospital Disaster Med 1990;5:59-63
163. Pepe P, Bonnin M, Almaquer D, Prentice F, Mattox K:
The effect of tiered system implementation on sudden death survival rates. Prehospital
Disaster Med 1989;4:71
164. Pepe P, Mattox K, Prentice F: Impact of full-time
physician supervision on an urban emergency medical services system (abstract). Prehospital
Disaster Med 1989;5:70
165. Pepe P, Copass M, Joyce T: Prehospital endotracheal
intubation – The rationale for training emergency medical personnel. Ann Emerg Med
1985;14:1085-1092
166. Newman MM: Early access, early CPR and early
defibrillation: Cry of the 1988 Conference on Citizen CPR. J Emerg Med Services 1988;13:30-35
167. Newman MM: Chain of Survival concept takes hold. J
Emerg Med Services 1989;14;11-13
168. Safar P, Bircher N: History and phases and stages of
cardiopulmonary cerebral resuscitation, in Safar P, Bircher N (eds): Cardiopulmonary
Cerebral Resuscitation, ed 3. Philadelphia, WB Saunders Co, 1988
169. Abramson N, Safar P, Detre K, Group BIS: Factors
influencing neurologic recovery after cardiac arrest (abstract). Ann Emerg Med 1989;18:477-478
170. Pepe P: Controlled studies in the prehospital
setting: A viable important venue for clinical research. Prehospital Disaster Med (in
press) |